Dive Brief:
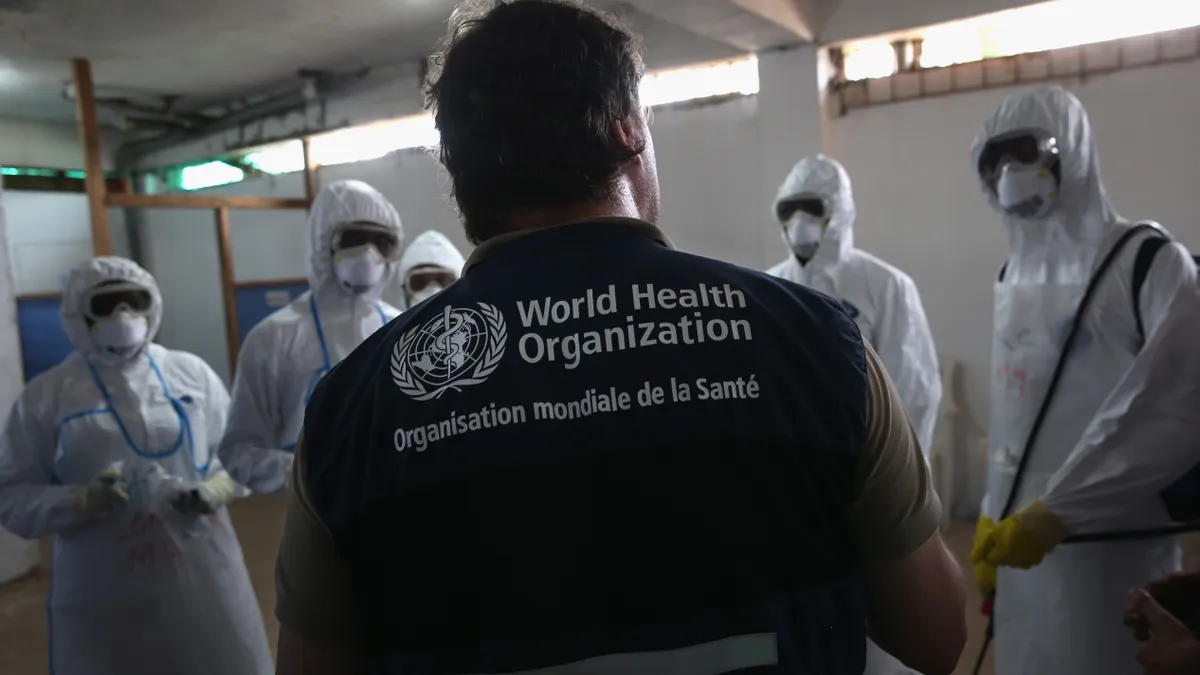
- The World Health Organization released on Sept. 3 its first-ever guidance regarding the reducing pollution caused by antibiotic manufacturing.
- The guidance sets health-based targets to protect humans and the environment from antimicrobial resistance risks, which occur when bacteria, viruses, fungi and parasites no longer respond to medicine.
- “Pharmaceutical waste from antibiotic manufacturing can facilitate the emergence of new drug-resistant bacteria, which can spread globally and threaten our health,” Dr. Yukiko Nakatani, the WHO assistant director-general for antimicrobial resistance ad interim, said in the agency’s release.
Dive Insight:
The WHO’s guidance looks to mitigate antibiotic resistance by managing wastewater and solid waste at pharmaceutical manufacturing sites.
Despite widespread documentation of pollution from water bodies downstream of antibiotic manufacturing sites, there is little regulation over emissions at these plants, the release stated. Additionally, environmental emissions are often not addressed in manufacturers’ quality assurance standards.
The guidance was developed after international bodies such as the WHO executive board, G7 health ministers and the United Nations Environment Programme called for an initiative to examine antibiotic production pollution.
The guidance covers all production process steps, from the manufacturing of active pharmaceutical ingredients and formulation into finished products, including primary packaging.
The WHO proposed different targets for antibiotic-resistant bacteria levels in solid waste, zero liquid discharge and wastewater.
For manufacturers, the agency suggests implementing risk management plans at each manufacturing site, including internal and external audits to ensure targets are progressively and consistently met.
The agency also suggests that manufacturers map their production systems and waste flows to identify areas with potential risks of antibiotic release. Additionally, manufacturers should publicly describe where responsibility lies in their antibiotic production supply chain, including where production occurs and how pollution is managed.
New Zealand was one example of a country making strides to reduce its production pollution. Authorities there provide full transparency on pharmaceutical supply chains by publishing detailed data, including company names and contact information for both active pharmaceutical ingredient production and formulation.
Elsewhere, in 2020, the India government proposed a bill to set pollution limits for antibiotics at manufacturing sites, but it passed without key discharge limits due to opposition from manufacturers.